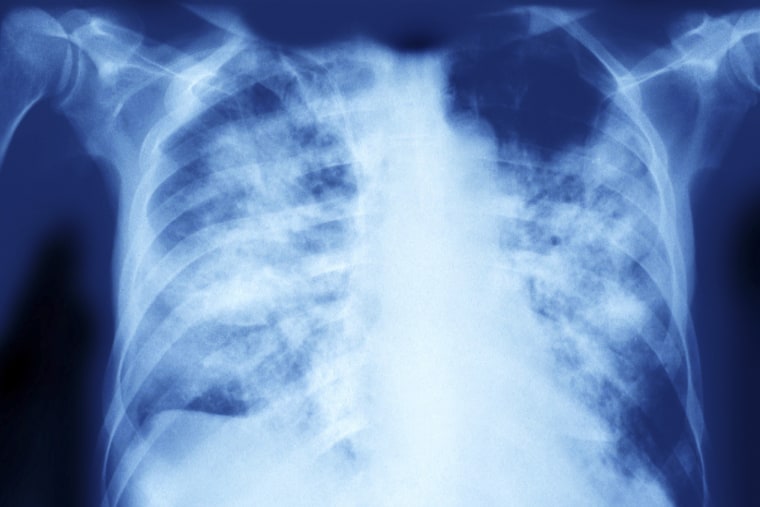
Franklin Dobbs, a 76-calendar year-aged patient of Pappas’, also experienced pre-present lung troubles in advance of he was identified with aspergillosis very last calendar year. Dobbs explained he hemorrhaged on and off for about a 12 months before getting identified. His circumstance has hence considerably not proved drug-resistant.
An azole referred to as Noxafil improved his indications, Dobbs reported, though he however feels weak.
“I’m even now obtaining a issue with the strength in my legs,” he mentioned.
Dobbs believes he could have been uncovered though planting tomatoes, corn and peas in the yard, or even though creating birdhouses outdoor.
An April review observed that persons can get infected with drug-resistant Aspergillus from their home gardens. The scientists gathered lung samples from contaminated people in the U.K. and Eire, and matched some of them to drug-resistant strains in the environments close by.
Often, a one high-dose publicity, this sort of as a cloud of spores released by digging in soil, can be plenty of to cause a fungal infection. But in numerous circumstances, people are gradually exposed to Aspergillus about months in advance of they grow to be unwell.
“This is an particularly concerning superbug-sort predicament,” Armstrong-James said. “We’re all inhaling this all the time. So probably, we could all be inhaling resistant Aspergillus on a daily foundation.”
Compared with Aspergillus, Candida auris is primarily detected in hospitals, amongst folks who are on respiratory or feeding tubes or acquiring a central line (an IV catheter that administers fluids, blood or medicine).
"When you have 1 of these health-related interventions that are in individuals, you develop into at possibility of it acquiring into your bloodstream or building an abscess, and which is when it’s pretty dangerous," explained Luis Ostrosky, chief of infectious ailments at UTHealth Houston and Memorial Hermann Healthcare facility.
Far more than 90% of Candida auris strains are resistant to the typical azole fluconazole, and up to 73% are resistant to a further known as voriconazole. Some strains also have resistance to the drug Fairweather not too long ago stopped getting.
"You can conclude up with a client with a Candida auris an infection the place you actually really do not have an antifungal to use for that affected person. It is resistant to every thing," Ostrosky said. "In essence individuals people go to hospice and die, and there’s nothing at all you can do."
Why mold is increasing resistant to medications
Scientists have pinpointed two most important drivers of antifungal resistance: human medication and chemicals made use of in agriculture.
Farmers normally depend on fungicides, but over time, particular strains of mildew grow to be resistant. And because fungicides are chemically related to antifungal prescription drugs, some mold strains establish resistance to the medicines way too.
The 65-year-old gentleman who died of invasive aspergillosis, for instance, was contaminated with a pressure connected to agricultural fungicide use, according to the CDC.
"Bulbs and onions that have been dipped in these antifungals so they really do not spoil are pretty much like time bombs. When they are planted, the fungicides that are on their surface will leak out into the natural environment," stated Armstrong-James, who co-authored the April examine on Aspergillus.
"That could be a crucial breeding floor for resistance," he extra.
Drug use contributes to resistance when antifungal prescription drugs are recommended way too often, or if health professionals you should not prescribe a superior plenty of dosage or long enough treatment study course. That can then place selective strain on fungi.
“The far more you use antifungals or antibacterials, the far more resistance that you see,” Pappas reported.
Armstrong-James explained that hospitals see resistance to Candida auris a lot more commonly than to Aspergillus.
"Each time everyone usually takes fluconazole, you can get Candida resistance," he mentioned.
Weather modify and Covid may just about every perform a part
Local weather improve may possibly be catalyzing the unfold of the two Aspergillus and Candida auris.
Which is mainly because mounting temperatures can guide to a lot more fungicide resistance. Some investigation indicates that local weather alter was a crucial driver of Candida auris’ first visual appeal in folks in 2009.
"Inside of a extremely limited period of time, you have bought the emergence of 4 or five various households of Candida auris extra or considerably less co-rising at the same time. How does that take place? It seriously screams if there’s a thing heading on in the setting," Pappas claimed. "There is first rate evidence that climate transform is at least one particular of the triggers."
Some authorities stress that as local weather change's outcomes intensify, even some balanced folks could get fungal infections.
"Even though there is no evidence for the instant that a completely properly person could get a severe Aspergillus infection, there’s nothing to say that, with the transforming environments, that may not change in the foreseeable future," Armstrong-James mentioned.
On leading of all this came the Covid pandemic, which developed new chances for Candida auris to distribute. A July CDC report found that these infections rose 60% in overall health treatment configurations from 2019 to 2020.
"Invasive Candida infections just skyrocketed with Covid, presumably due to the fact all these patients have been ill," Pappas stated. "They ended up supplied broad spectrum antibiotics. They experienced lines and ventilators and all the points that you require to crank out invasive Candida."
The CDC report located that staffing shortages and prolonged affected individual stays, amid other elements, manufactured it tricky for some hospitals to avert drug-resistant infections.
"We were being having all these traveling nurses that came from diverse areas of the region that weren’t necessarily attuned to the protocols that the healthcare facility usually has to avoid bloodstream bacterial infections," Ostrosky mentioned.

New procedure options could take several years
Medical practitioners say they're in a race versus time, because latest therapies could quit performing right before new ones grow to be obtainable.
“If we really don't deal with resistance ideal now and if we never strengthen the pipeline for the antifungals, we could quite conveniently conclude up in a position in 5 to 10 many years where by you’re possessing close-of-lifestyle conversations with a affected person that has an invasive Candida infection," Ostrosky explained. "It is just unthinkable correct now that your liked a single can go into the hospital and have an appendectomy, and they get a complication, and they finish up with a bug that’s untreatable."
A number of drugs have entered late-phase studies that could create effects in the future 12 months or two, industry experts said.
But Fairweather isn’t confident she’ll get a chance to try out them.
"How significantly injury will be accomplished to my lungs prior to these items occur into result?" she said.
Moreover, fungi could build resistance to new medicines around time.
"As soon as they are out there, they get overused and then fairly rapidly, they are no more time useful," Pappas claimed.
[ad_2]





0 comments:
Post a Comment